The New World Of Laboratory Medicine
Yesterday I listened to a very interesting webinar by Richard Friedberg, MD PhD, Professor and Deputy Chairman of the Department of Pathology, Tufts University School of Medicine, Boston, MA. Dr Friedberg is also Chairman of the Pathology for Baystate Health (Springfield, MA), where he oversees a 22-pathologist academic/private practice operation responsible for 50,000 surgical specimens, 90,000 cytology specimens, 6 million laboratory tests, and a large reference laboratory.
As a pathologist myself, I had been looking forward to hearing him speak. Some of the highlights from Dr Friedberg’s webinar are outlined below:
The Evolution Of Pathology
Dr Friedberg reviewed how laboratory medicine and the practice of pathology have evolved over the decades, and how they are likely to continue to evolve in the future. Pathology has changed in numerous ways, involving a move from a formerly qualitative and later quantitative approach, to a more integrative approach currently. Additionally, our specialty has moved from “analog” to “digital”, similar to what has occurred in the field of radiology.
He talked about how, in order to thrive in highly competitive markets, clinical laboratories need to look beyond traditional models of service delivery and must now think outside the box. This may mean integrating with other diagnostic services and delivering different types of results (from laboratory to imaging) to physicians and other clients. Traditionally, “pathology” and “imaging” have been considered separate entities, but the trend is definitely moving toward a more integrated approach of diagnostic reporting that incorporates both disciplines.
Therefore, in coming years, a diagnostic report will be much more than the traditional “label” of the past. Changes including the advancement of personalized medicine, the use of electronic medical records, and the evolution of technological advancements like digital pathology, will all impact how pathologists work. Consequently the pathologist’s report will no longer merely comprise a diagnostic name, but rather will represent an aggregate of much medical information that has been analysed using disparate tools.
The Downside Of Digitization
Some professionals have been concerned that the improvement by “moving to digital” might also have a negative effect – namely the outsourcing of pathology to overseas countries for low cost services (as has occurred in the field of radiology); however, this may not be as much of a cause for concern in pathology, for a few reasons:
Initial Image Capture: Radiological images are first obtained digitally. This is not the case with microscopic images though – the need for initial slide production will always remain. So there will always remain the need for a laboratory system to process the sample and subsequently generate the digital image from the specimen.
Image File Size: File sizes of microscopic images are much larger than radiological images, and therefore not quite as easy to forward.
Urgency: Digital forwarding of radiological images to an overseas specialist for immediate consultation has important implications in medicine. It might, for example, allow a patient in the ER to be appropriately treated or released within minutes of an imaging procedure. With surgical biopsy specimens that require routine processing, however, this urgency tends not to exist. This process is indeed still constrained by the typical turnover time of up to 24 hours or more that is required to optimally process a specimen (from formalin fixation, until a hematoxylin and eosin-stained slide is produced).
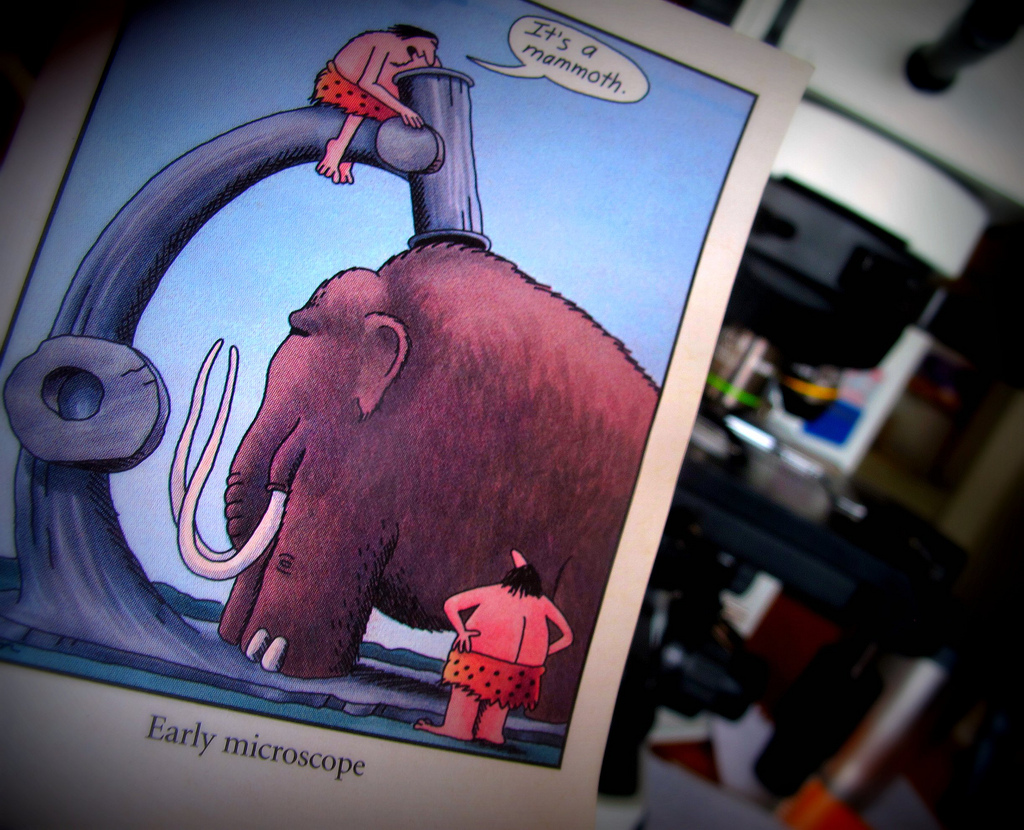 |
| “It’s A Mammoth” |
The Tyranny Of The Tool
It is important to remember that through the centuries, pathologists have traditionally made careers out of recognizing patterns. The more recent evolution of pathology, however, means that we can no longer allow ourselves to be merely defined by our tool, the microscope. Does your job involve you working as a microscopist, or a diagnostician? Moving forward, it is most important to be the latter. We must begin to learn new ways of thinking and working in our professional environment, otherwise, allowing ourself to be defined solely by a microscope could put us out of business!
In A Nutshell
The most important thing is that we know a transition phase in pathology reporting is underway – we just don’t exactly know how long it will take. This leaves plenty of professionals currently trying to figure out where they might stand in this new, evolving healthcare approach. As pathologists, we must therefore prepare for tomorrow, and position ourselves firmly, using all the diagnostic skills we can offer in addition to microscopy.
And although the future of pathology provides a definite challenge for us all, it should, nevertheless, be a fascinating and enjoyable ride!